APrf Martin Donnelley
Externally-Funded Research Fellow (D)
School of Medicine
College of Health
Eligible to supervise Masters and PhD - email supervisor to discuss availability.
I am an Associate Professor at Adelaide University, Leader of the Respiratory X-ray Imaging Laboratory (ReXIL), Director of the Cystic Fibrosis Airway Research Group (CFARG) at the Women’s and Children’s Hospital in Adelaide, and the Robinson Research Institute Research Leadership Co-Lead for Developmental Disorders.
I completed my PhD in Medical Image Processing at the Flinders University of South Australia in 2008, and have spent the last ~20 years developing world-leading gene therapy methodologies, as well as technologies for the measurement of in vivo dynamic function in animal models. I am therefore in the unique position of having split the focus of my career equally on the fields of X-ray imaging and cystic fibrosis (CF) gene therapy, with the goal of using my advances in imaging to substantially improve outcomes in CF.
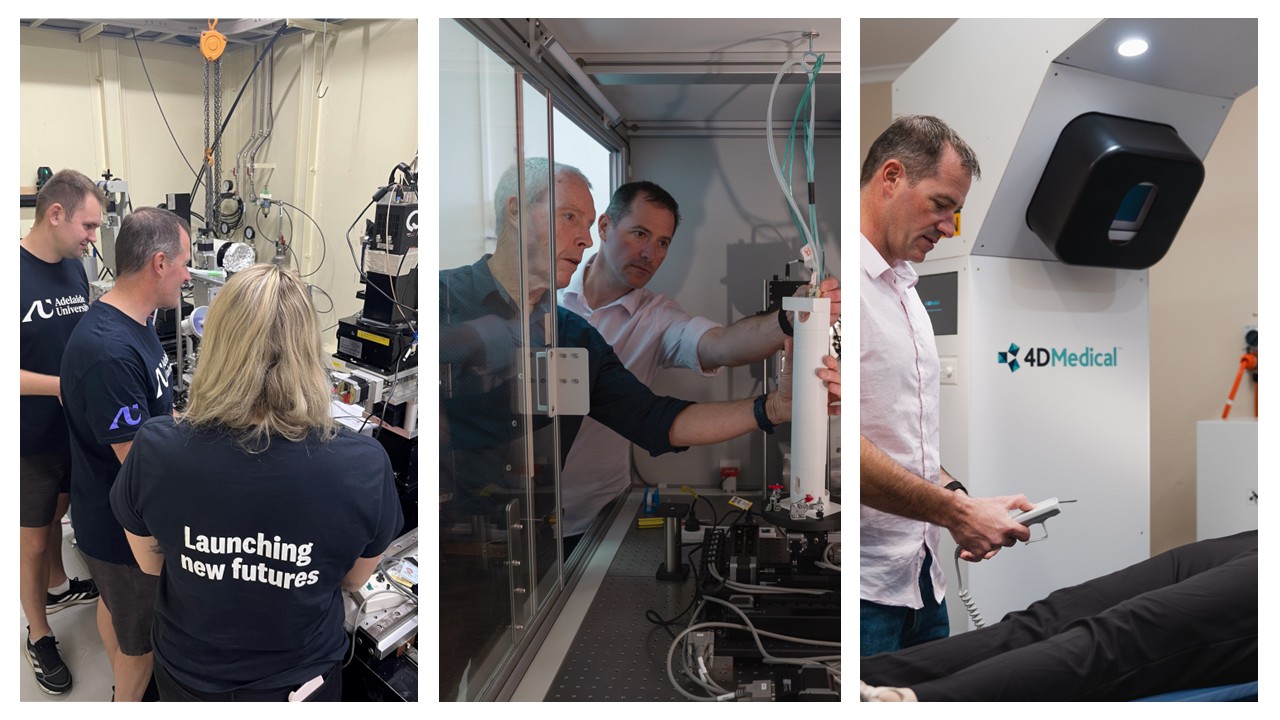
As the ReXIL Leader I have directed a program of X-ray imaging work that has enabled the imaging of respiratory processes at scales that have not previously been possible in vivo. I have developed a novel non-invasive airway health assessment method based on using synchrotron imaging to track changes in the mucociliary transit (MCT) behaviour of deposited marker particles following pharmaceutical treatments. This work is linked to studies I performed with collaborator A/Prof Kaye Morgan (Monash University), that show we can also measure changes in airway surface liquid (ASL) depth in live anaesthetised mouse airways. We have now combined these methods into a single powerful airway health assessment method. In 2016 my collaborators and I published the first demonstration of the use of X-ray Velocimetry (XV), an X-ray based pulmonary function testing for the quantification of lung disease heterogeneity in B-ENaC mice. This unique and world-leading imaging method gathers lung motion information during normal breathing, and has revolutionary potential since it can detect, quantify and follow changes in regional lung function over time. I now have industry collaborations with 4DMedical (Prof Andreas Fouras) who have commercialised this technology. This work has been funded by the NHMRC, MRFF and AEA. In 2023 my team won the Australian Museum Eureka Prize for Interdisciplinary Scientific Research for our work on developing and applying X-ray Velocimetry for CF.
In 2014 my CFARG team published key data to show that our airway conditioning and lentiviral gene vector system produces correction of the CFTR defect in CF mouse nasal airways for at least 12 months. This work was the first to show improved survival in the gene vector treated CF group, supporting the prediction that CF airway gene therapy can produce significant health benefits. In 2017 I championed the development of Adelaide-based CF rat models using CRISPR/Cas9 gene editing, to facilitate further development of my group's airway gene therapy. The phenotype characterisation of these models was published in 2020. We now have CF rats and B-ENaC mice available for studies in Adelaide.
I am a world leader in dynamic imaging for lung disease, and aim to develop CF airway gene therapy to the point that it can be translated into a clinical tool. My strategy is based on utilising a combination of world-leading technologies; a proven gene vector, the right animal models, and a suite of X-ray imaging techniques for assessing lung function and airway surface health to radically boost the health outcomes of children and adults with CF.
Respiratory X-ray Imaging Laboratory (ReXIL)
ReXIL aims to develop rapid and accurate outcome measures for assessment of airway disease using X-ray imaging. We have access to the SPring-8 Synchrotron in Japan and the Australian Synchrotron in Melbourne, as well as local X-ray imaging facilities at the SAHMRI PIRL facility at Gilles Plains. This enables us to image at a range of scales from micro through to macro, using small and large animal models. Our Honours and HDR projects focus on algorithm development for X-ray Velocimetry (XV) and synchrotron-acquired data. We also use our cystic fibrosis rat and mouse (B-ENaC) models for evaluation of therapies. Some of these studies involve work with our Melbourne-based industry partner 4DMedical.
Cystic Fibrosis Airway Research Group (CFARG)
The CFARG goals are to better understand the role of lung fibrosis in cystic fibrosis disease development, and to develop an effective genetic or cell-based therapy for prevention or treatment of Cystic Fibrosis airway disease. Our research themes are currently focussed on several complementary areas; achieving effective lentiviral CFTR vector gene delivery, lentiviral vector development, upscaling vector production, transducing airway stem cells in situ to enable extended gene expression, and creating and testing new delivery methods. We have access to a range of animal models (including CF mice and rats, and large animals), and a dedicated state-of-the-art research laboratory in Respiratory Medicine at the Women's and Children's Hospital. Our Honours, Masters and PhD projects can be tailored to focus on any aspect of this work, and may be related to gene therapy studies in CF rats, assessment of in vivo gene expression, stem cell analyses including FACS analyses, and LV vector production improvements.
Example projects include, but are not limited to:
Project 1
Title: Demonstrating the effectiveness of gene therapy for altering CF-related lung and airway health in CF rat lungs
Description: An effective gene-addition therapy for CF lung disease requires accurate compound delivery to the target location, high levels of transduction, and effective CFTR protein expression in the cells relevant to CF disease. The aim of this project is to determine whether CFTR gene-addition alters the course of lung disease in our CF rat models, visualise the location of the transduced cells, and quantify how much expression is produced. This will be achieved with the use of tools such as PCR, histology, immunohistochemistry, and nasal potential difference assessment, as well as gene vector production.
Co-supervisor(s): Dr Alexandra McCarron, Dr Nikki Reyne
Projects available for: Honours, Masters and PhD
Location: Women’s and Children’s Hospital
Research project start: Semester 1 or 2
Special Requirements: None
Project 2
Title: Turning X-ray Velocimetry lung motion data into clinical impact
Description: X-Ray Velocimetry (XV)is a revolutionary lung imaging technology developed by Australian company 4DMedical. XV enables lung motion to be tracked over time, and airflow to be calculated at any point in the airway tree. This allows the location and intensity of lung disease, and its resolution with treatment, to be measured. The aim of this project is to develop algorithms for analysing XV data, create predictive models for disease progression, and identify patterns in imaging data that correlate with clinical outcomes.
Co-supervisor(s): Dr Ronan Smith, Dr Nikki Reyne, Dr Dhani Dharmaprani (Flinders)
Projects available for: Honours, Masters and PhD
Location: Women’s and Children’s Hospital
Research project start: Semester 1 or 2
Special Requirements: Significant knowledge of machine learning techniques required.
Project 3
Title: Measurement of lung function and airway surface health
Description: The ability to rapidly and accurately measure the effects of genetic or pharmaceutical therapies on airway surface health and lung function are very important. We have developed X-ray imaging technologies to quantify treatment efficacy.
The ability to image ciliary action has significant clinical relevance, as disruptions in ciliary function are hallmarks of several respiratory diseases. At the SPring-8 synchrotron in Japan we can measure changes in the ciliary beat using and approach called directional dark field (DDF) imaging. DDF X-ray imaging is a powerful new technique that enhances contrast by selectively detecting X-rays scattered at specific angles, making it particularly well-suited for visualizing fine, dynamic structures like motile cilia. The development and application of DDF techniques is a key focus of our collaborators at the Monash University Physics of X-ray Imaging Group (PhIG). In recent studies at the Australian Synchrotron’s Imaging and Medical Beamline (IMBL) we have also used DDF imaging to examine ventilation defects in a model of CF lung disease (B-ENaC mouse) and a mouse model of lung cancer, and from ventilator-induced lung injury.
These projects are designed to develop and apply DDF approaches to medical data. Depending on the expertise, skills and interests of the applicant it could involve computer science techniques such as image processing algorithm development and image data analysis, or alternatively it could be based on animal handling and molecular assessments.
Co-supervisor(s): Dr Ronan Smith, Dr Nikki Reyne
Projects available for: Honours, Masters and PhD
Location: Women’s and Children’s Hospital
Research project start: Semester 1 or 2
Special Requirements: Some travel may be involved.
| Date | Position | Institution name |
|---|---|---|
| 2023 - ongoing | Associate Professor | University of Adelaide |
| 2019 - ongoing | Research Leader | Robinson Research Institute |
| 2018 - 2022 | Senior Research Fellow | University of Adelaide |
| 2018 - 2018 | Career Development Fellow | Robinson Research Institute |
| 2016 - 2017 | Affiliate Senior Lecturer | University of Adelaide |
| 2007 - 2017 | Senior Medical Scientist | Women's and Children's Hospital |
| Date | Type | Title | Institution Name | Country | Amount |
|---|---|---|---|---|---|
| 2023 | Award | Australian Museum Eureka Prize for Interdisciplinary Scientific Research | Australian Museum | Australia | - |
| 2018 | Fellowship | Robinson Research Institute Career Development Fellowship | University of Adelaide | Australia | - |
| 2017 | Award | Translational Research Award | Women's and Children's Health Network Service Excellence Awards | Australia | - |
| 2013 | Fellowship | MS McLeod Postdoctoral Research Fellowship | Women's and Children's Hospital | Australia | - |
| 2009 | Award | Semi-finalist for Young Investigator Award | Women's and Children's Hospital | Australia | - |
| Date | Institution name | Country | Title |
|---|---|---|---|
| 2002 - 2007 | Flinders University | Australia | PhD |
| 1997 - 2000 | Flinders University | Australia | BSc |
| 1997 - 2001 | Flinders University | Australia | BEng (Biomedical) with Honours (First Class) |
| Year | Citation |
|---|---|
| 2025 | Bruorton, M., Phillips, J., Donnelley, M., Goddard, T., O'Connor, A., Parsons, D., . . . Tai, A. (2025). Visualizing Lung Ventilation Heterogeneity in Children With X-ray Velocimetry. In AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE Vol. 211 (pp. 1 page). CA, San Francisco: AMER THORACIC SOC. DOI |
| 2025 | Davis, M., McCarron, A., Smith, R., Rout-Pitt, N., Reyne, N., Costello, L., . . . Donnelley, M. (2025). Optimising Magnetic-Guidance of Lentiviral Vectors for Improved Airway Gene Therapy Efficacy. In MOLECULAR THERAPY Vol. 33 (pp. 2 pages). LA, New Orleans: CELL PRESS. |
| 2024 | Grunert, J., Zanardo, G., Johnston, J., Donnelley, M., & Tai, A. (2024). Nutritional outcomes in adolescent patient with CF after 12 months of Elexacafor/Tezacaftor/Ivacaftor (ETI) (Trikafta<SUP>®</SUP>) therapy. In RESPIROLOGY Vol. 29 (pp. 38). WILEY. |
| 2024 | Johnston, J., Donnelley, M., & Tai, A. (2024). Clinical outcomes in a 12-18 year old cystic fibrosis cohort following commencement of Elexacaftor/ Tezacaftor/Ivacaftor: A retrospective, single-centre audit. In RESPIROLOGY Vol. 29 (pp. 163). WILEY. |
| 2024 | Reyne, N., Cmielewski, P., Smith, R., Eikelis, N., Nilsen, K., Mall, M., . . . Donnelley, M. (2024). X-ray Velocimetry detects peripheral lung ventilation defects in ßENaC mice. In RESPIROLOGY Vol. 29 (pp. 166). WILEY. |
| 2024 | Bruorton, M., Carson-Chahhoud, K., Donnelley, M., Goddard, T., O'Connor, A., Parsons, D., . . . Tai, A. (2024). Feasibility study of x-ray Velocimetry imaging in children with CF. In RESPIROLOGY Vol. 29 (pp. 225). WILEY. |
| 2023 | dos Reis, D. C., Dastoor, P. K., Santos, A. K., Cohen, M. B., Donnelley, M., & Ameen, N. A. (2023). ROLE OF CFTR HIGH EXPRESSOR CELLS (CHES) IN CYSTIC FIBROSIS INTESTINAL DISEASE. In GASTROENTEROLOGY Vol. 164 (pp. S225). IL, Chicago: W B SAUNDERS CO-ELSEVIER INC. |
| 2022 | Drysdale, V., Cmielewski, P., Donnelley, M., Parsons, D., Reyne, N., & McCarron, A. (2022). Miniature Devices for Controlled Airway Surface Perturbation in Rats: Which Device Produces the Best Lentiviral Vector Gene Transfer?. In MOLECULAR THERAPY Vol. 30 (pp. 284). CELL PRESS. |
| 2022 | Donnelley, M., Cmielewski, P., Morgan, K., Delhove, J., Reyne, N., McCarron, A., . . . Parsons, D. (2022). In Vivo Lentiviral Gene Transfer to Airway Surfaces for Cystic Fibrosis is Improved by Magnetic Guidance of Particles. In MOLECULAR THERAPY Vol. 30 (pp. 421). CELL PRESS. |
| 2021 | Reyne, N., Cmielewski, P., McCarron, A., Parsons, D., & Donnelley, M. (2021). Lentiviral Airway Gene Therapy Correction of CFTR Function in Knockout Cystic Fibrosis Rats. In MOLECULAR THERAPY Vol. 29 (pp. 259). CELL PRESS. |
| 2021 | Reyne, N., Cmielewski, P., Mccarron, A., Parsons, D., & Donnelley, M. (2021). LENTIVIRAL AIRWAY GENE-ADDITION CORRECTS CF RAT NASAL ION CHANNEL FUNCTION. In RESPIROLOGY Vol. 26 (pp. 156). WILEY. |
| 2021 | Jayapal, M., Tran H, B., Maiolo, S., Reynolds, P., Liu, H., Parsons, D., . . . Hodge, S. (2021). PYOCYANIN INCREASES VASCULAR RAC1/ZIP12/BMPR2-RELEVANCE TO VASCULAR DYSFUNCTION AND REMODELLING IN CYSTIC FIBROSIS. In RESPIROLOGY Vol. 26 (pp. 59). WILEY. |
| 2019 | Gardner, M., Donnelley, M., Parsons, D., Morgan, K., McCarron, A., & Cmielewski, P. (2019). Neural Networks provide superior detection of particles in Synchrotron X-ray images for automated Mucociliary Transport measurement. In 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). online: IEEE. |
| 2019 | Parsons, D., Cmielewski, P., Mccarron, A., Mcintyre, C., Craig, F., Finnie, J., . . . Donnelley, M. (2019). Update on the Australian cystic fibrosis rat colony. In Respirology Vol. 24 (pp. 136). Broadbeach, Qld.: Wiley. |
| 2019 | Macowan, M., Tran, H., Matthews, K., Ralph, M., Donnelley, M., Parsons, D., & Hodge, S. (2019). DYSREGULATED S1P SIGNALLING IN MOUSE MODEL OF CYSTIC FIBROSIS-LIKE LUNG DISEASE PRODUCED BY βENAC OVEREXPRESSION. In RESPIROLOGY Vol. 24 (pp. 118). WILEY. |
| 2019 | McCarron, A., Donnelley, M., Cmielewski, P., McIntyre, C., & Parsons, D. (2019). Transient Lentiviral Vector Production Using a Packed-Bed Bioreactor System. In MOLECULAR THERAPY Vol. 27 (pp. 209). Washington, DC: CELL PRESS. |
| 2019 | Morgan, K. S., Gradl, R., Dierolf, M., Jud, C., Günther, B., Werdiger, F., . . . Donnelley, M. W. (2019). In vivo x-ray imaging of the respiratory system using synchrotron sources and a compact light source. In B. Müller, & G. Wang (Eds.), Developments in X-Ray Tomography XII Vol. 11113 (pp. 111130G-1-111130G-12). online: Society of Photo-optical Instrumentation Engineers. DOI Scopus1 |
| 2019 | Li, J., Quirk, B. C., Delhove, J., Kirk, R., Mc Carron, A., Cmielewski, P., . . . McLaughlin, R. A. (2019). Imaging genetically-modified cells with a miniaturised multimodal optical coherence tomography + fluorescence probem. In Proceedings of the 2019 IEEE Photonics Conference (IPC) (pp. 1-2). Piscataway, NJ: IEEE. DOI Scopus1 WoS1 |
| 2018 | Gradl, R., Dierolf, M., Hehn, L., Gunther, B., Kutschke, D., Yang, L., . . . Morgan, K. (2018). Dynamic x-ray imaging at the Munich Compact Light Source. In Microscopy and Microanalysis Vol. 24 (pp. 350-351). Saskatoon, Canada: MIcroscopy Society of America. DOI |
| 2017 | Jung, H., Lee, I., Lee, S., Parsons, D., & Donnelley, M. (2017). Multiple mucociliary transit marker tracking in synchrotron X-ray images using the global nearest neighbor method. In Proceedings of the 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC' 17) Vol. 2017 (pp. 1824-1827). Online: IEEE. DOI Scopus2 WoS3 |
| 2016 | McCarron, A., McIntyre, C., Donnelley, M., Cmielewski, P., & Parsons, D. (2016). Development of a Clinically-Acceptable Lentiviral Vector for Cystic Fibrosis Airway Gene Therapy. In MOLECULAR THERAPY Vol. 24 (pp. S280-S281). Washington, DC: NATURE PUBLISHING GROUP. DOI |
| 2016 | Donnelley, M., Morgan, K., Farrow, N., Siu, K., & Parsons, D. (2016). Non-invasive airway health measurement using synchrotron X-ray microscopy of high refractive index glass microbeads. In M. D. DeJonge, D. J. Paterson, & C. G. Ryan (Eds.), Aip Conference Proceedings Vol. 1696 (pp. 4 pages). Australian Synchrotron, Melbourne, AUSTRALIA: AMER INST PHYSICS. DOI Scopus8 WoS6 |
| 2012 | Morgan, K., Paganin, D., Parsons, D., Donnelly, M., Yagi, N., Uesugi, K., . . . Siu, K. (2012). Single grating x-ray imaging for dynamic biological systems. In International Workshop on X-Ray and Neutron Phase Imaging with Gratings Vol. 1466 (pp. 124-129). United States: Springer New York LLC. DOI Scopus3 WoS3 |
| 2010 | Donnelley, M., Parsons, D., Morgan, K., & Siu, K. (2010). Animals In synchrotrons: overcoming challenges for high-resolution, live, small-animal imaging. In K. Siu (Ed.), Proceedings of 6th International Conference on Medical Applications of Synchrotron Radiation Vol. 1266 (pp. 30-34). United States: American Institute of Physics. DOI Scopus19 WoS14 |
| 2009 | Donnelley, M., Badiei, A., Cleek, T., Bottema, M., Fazzalari, N., & Reynolds, K. (2009). Cortical thickness changes in rat tibiae: The effect of Ovx and bisphosphonate treatment. In BONE Vol. 44 (pp. S134-S135). Sydney, AUSTRALIA: ELSEVIER SCIENCE INC. DOI |
| 2009 | Morgan, K., Paganin, D., Parsons, D., Donnelley, M., Yagi, N., Uesugi, K., . . . Siu, K. (2009). Optimising coherence properties for phase contrast x-Ray imaging (PCXI) to reveal airway surface liquid (ASL) as an airway health measure. In Ifmbe Proceedings Vol. 25 (pp. 135-138). Munich, Germany: Springer Verlag. DOI Scopus2 WoS2 |
| 2008 | Donnelley, M., Knowles, G., & Hearn, T. (2008). A CAD system for long-bone segmentation and fracture detection. In A. Elmoataz, O. Lezoray, F. Nouboud, & D. Mammass (Eds.), Lecture Notes in Computer Science Including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics Vol. 5099 LNCS (pp. 153-162). Cherbourg-Octeville, FRANCE: SPRINGER-VERLAG BERLIN. DOI Scopus20 WoS15 |
| 2005 | Donnelley, M., & Knowles, G. (2005). Automated bone fracture detection. In J. M. Fitzpatrick, & J. M. Reinhardt (Eds.), Progress in Biomedical Optics and Imaging Proceedings of SPIE Vol. 5747 (pp. 955-966). San Diego, CA: SPIE-INT SOC OPTICAL ENGINEERING. DOI Scopus7 WoS3 |
| 2005 | Donnelley, M., & Knowles, G. (2005). Computer aided long bone fracture detection. In Proceedings 8th International Symposium on Signal Processing and Its Applications Isspa 2005 Vol. 1 (pp. 175-178). Sydney, AUSTRALIA: IEEE. DOI Scopus10 WoS9 |
| 2002 | Gopalakrishnan, D., McLennan, G., Donnelley, M., Delsing, A., Suter, M., Flaherty, D., . . . Reinhardt, J. M. (2002). Color analysis of the human airway wall. In A. N. Clough, & C. T. Chen (Eds.), Proceedings of SPIE the International Society for Optical Engineering Vol. 4683 (pp. 341-351). CA, SAN DIEGO: SPIE-INT SOC OPTICAL ENGINEERING. DOI Scopus2 WoS2 |
| Year | Citation |
|---|---|
| 2024 | Parsons, D., Bruorton, M., Phillips, J., Eikelis, N., Nilsen, K., Carson-Chahoud, K., . . . Goddard, T. (2024). Lung ventilation via x-ray velocimetry imaging and PFTs in CF children: Case-studies from the ongoing Adelaide pilot and feasibility trial. Poster session presented at the meeting of Abstracts of The Australia & New Zealand Society of Respiratory Science and The Thoracic Society of Australia and New Zealand (ANZSRS/TSANZ) Annual Scientific Meeting for Leaders in Lung Health & Respiratory Science (TSANZSRS 2024), as published in Respirology. Gold Coast Convention and Exhibition Centre, Gold Coast, QLD: Wiley. DOI |
| 2024 | Reyne, N., Cmielewski, P., Smith, R., Eikelis, N., Nilsen, K., Christou, C., . . . Donnelley, M. (2024). Comparing lung ventilation using x-ray velocimetry across various mammals. Poster session presented at the meeting of Abstracts of the The Australia & New Zealand Society of Respiratory Science and The Thoracic Society of Australia and New Zealand (ANZSRS/TSANZ) Annual Scientific Meeting for Leaders in Lung Health & Respiratory Science (TSANZSRS 2024), as published in Respirology. Gold Coast Convention and Exhibition Centre, Gold Coast, QLD: Wiley. DOI |
| 2024 | Li, D., Donnelley, M., Parson, D., Habgood, M., & Schneider-Futschik, E. (2024). Late pregnancy Elexacaftor/Tezacaftor/ Ivacaftor exposure may harm developing thymus and cortex. Poster session presented at the meeting of Abstracts of the Australia & New Zealand Society of Respiratory Science and The Thoracic Society of Australia and New Zealand (ANZSRS/TSANZ) Annual Scientific Meeting for Leaders in Lung Health & Respiratory Science (TSANZSRS 2024), as published in Respirology. Gold Coast Convention and Exhibition Centre, Gold Coast, QLD: Wiley. DOI |
| 2023 | Rout-Pitt, N., Mc Carron, A., Boog, B., Parsons, D., & Donnelley, M. (2023). A twist in the cystic fibrosis story—TGF-β1 treatment affects epithelialmesenchymal transition differentially in two cystic fibrosis rat airway cell models. Poster session presented at the meeting of North American Cystic Fibrosis Conference. |
| 2023 | Li, D., Habgood, M., Reyne, N., Cmielewski, P., McCarron, A., Parsons, D., . . . Schneider-Futschik, E. (2023). Cystic fibrosis modulator triple combination in pregnancy and lactation: Effects on the developing lung, gut and pancreas. Poster session presented at the meeting of Abstracts of The Australia & New Zealand Society of Respiratory Science and The Thoracic Society of Australia and New Zealand (ANZSRS/TSANZ) Annual Scientific Meeting for Leaders in Lung Health & Respiratory Science (TSANZSRS, 2023) as published in Respirology. Christchurch, Aotearoa New Zealand: Wiley. DOI |
| 2023 | Roff, A. J., Robinson, J. L., Hammond, S. J., Davies, A., Clifton, V. L., Wallace, M. J., . . . Donnelley, M. (2023). X-ray Velocimetry Detects Changes in Local Airflow in a Sheep Model of Asthma During Pregnancy. Poster session presented at the meeting of REPRODUCTIVE SCIENCES. Germany: SPRINGER HEIDELBERG. |
| 2023 | Smalley, E. K., Song, Y., Dubsky, S., Trevascus, D., Preissner, M., Morgan, K., . . . Zosky, G. R. (2023). Alteration of PEEP Impacts End-expiratory Volume Variability and May Promote Ventilator Induced Lung Injury. Poster session presented at the meeting of Abstracts of the International Conference of the American Thoracic Society (ATS 2023), as published in the American Journal of Respiratory and Critical Care Medicine. DC, Washington: American Thoracic Society. DOI |
| 2022 | Reyne, N., Cmielewski, P., Boog, B., McCarron, A., Parsons, D., & Donnelley, M. (2022). Cystic fibrosis rat models demonstrate altered respiratory mechanics. Poster session presented at the meeting of Abstracts of the The Australia & New Zealand Society of Respiratory Science and The Thoracic Society of Australia and New Zealand (ANZSRS/TSANZ), Annual Scientific Meeting for Leaders in Lung Health & Respiratory Science (TSANZSRS, 2022), as published in Respirology. virtual online: Wiley. DOI |
| 2021 | Tran, H., Jayapal, M., Donnelley, M., Parsons, D., & Parsons, D. (2021). MECHANISMS LEADING TO PULMONARY VASCULAR DISORDERS MAY ARISE BEFORE FULL PENETRATION OF LUNG DISEASE IN CF RATS. Poster session presented at the meeting of RESPIROLOGY. WILEY. |
| 2020 | Reyne, N., Cmielewski, P., McCarron, A., Parsons, D., & Donnelley, M. (2020). Measuring CFTR Function in CF Rats: Optimisation of the Nasal Potential Difference Technique. Poster session presented at the meeting of Abstracts of the the 34th Annual North American Cystic Fibrosis Conference (NACFC 2020), as published in Pediatric Pulmonology. Phoenix, Arizona and virtual online: Wiley. DOI |
| 2020 | Delhove, J., Donnelley, M., & Parsons, D. (2020). ENGINEERING IMMUNE STEALTH, STEM CELL-TARGETING LENTIVIRAL VECTORS FOR CYSTIC FIBROSIS GENE THERAPY. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY. |
| 2020 | McCarron, A., Farrow, N., Cmielewski, P., Reyne, N., Parsons, D., & Donnelley, M. (2020). AIRWAY GENE-ADDITION THERAPY FOR CF LUNG DISEASE: STRATEGIES FOR IMPROVING GENE TRANSFER EFFICACY AND LONGEVITY. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY. |
| 2020 | Dusting, J., Donnelley, M., Parsons, D., & Fouras, A. (2020). DEDICATED XV HUMAN SCANNER DELIVERING 4D REGIONAL LUNG FUNCTION ANALYSIS WITH A LOWER DOSE THAN CHEST X-RAY. Poster session presented at the meeting of RESPIROLOGY. WILEY. |
| 2020 | Delhove, J., Donnelley, M., & Parsons, D. (2020). Generation of Immune Resistant, Stem Cell Targeting Lentivirus for Cystic Fibrosis Airway Gene Therapy. Poster session presented at the meeting of MOLECULAR THERAPY. ELECTR NETWORK: CELL PRESS. |
| 2020 | Rout-Pitt, N., Delhove, J., Farrow, N., Donnelley, M., & Parsons, D. (2020). Development of an Epithelial Mesenchymal Transition Tracing Vector. Poster session presented at the meeting of MOLECULAR THERAPY. ELECTR NETWORK: CELL PRESS. |
| 2020 | Carpentieri, C., Farrow, N., Cmielewski, P., Delhove, J., Rout-Pitt, N., Parsons, D., & Donnelley, M. (2020). Frequency and Timing of Lentiviral Vector Repeat Dose Delivery Does Not Significantly Alter Long-Term Transgene Expression Levels in Mouse Lungs. Poster session presented at the meeting of MOLECULAR THERAPY. ELECTR NETWORK: CELL PRESS. |
| 2020 | Carpentieri, C. L., Cmielewski, P., McCarron, A., Reyne, N., Boog, B., Farrow, N., . . . Parsons, D. (2020). ACUTE PSEUDOMONAS AERUGINOSA INFECTION IN WILD-TYPE AND PHE508DEL CF RATS. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY. |
| 2019 | Tran, H. B., Macowan, M., Abdo, A., Donnelley, M., Parsons, D., & Hodge, S. (2019). Airway inflammasome activation and dysregulated S1P signalling associated with mucus obstruction in a cystic fibrosis-like mouse model.. Poster session presented at the meeting of Respirology. Wiley. |
| 2019 | Cmielewski, P., McCarron, A., Reyne, N., Finnie, J., Rout-Pitt, N., Schjenken, J., . . . Donnelley, M. (2019). AN UPDATE ON THE PHENOTYPE CHARACTERISATION OF PHE508DEL AND CFTR KNOCKOUT RATS. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY. |
| 2019 | Werdiger, F., Morgan, K. S., Dusbky, S., Cmielewski, P., Kitchen, M., Klein, M., . . . Donnelley, M. (2019). Quantification of local lung disease in rat models of CF disease and CF knockout mice. Poster session presented at the meeting of Pediatric Pulmonology. Nashville, Tennessee: Wiley. |
| 2019 | Rout-Pitt, N., Donnelley, M., & Parsons, D. (2019). OPTIMISATION OF BRONCHOSCOPIC LENTIVIRAL VECTOR DELIVERY FOR DIRECT LOBE TARGETING IN RAT LUNGS. Poster session presented at the meeting of RESPIROLOGY. WILEY. |
| 2019 | Donnelley, M., Osenk, I., Delhove, J., & Prichard, I. (2019). A Systematic Review of the Public Acceptability of Gene Therapy and Gene Editing for Human Applications. Poster session presented at the meeting of MOLECULAR THERAPY. Washington, DC: CELL PRESS. |
| 2019 | Farrow, N., Carpentieri, C., Delhove, J., Rout-Pitt, N., Parsons, D., & Donnelley, M. (2019). ASSESSING LENTIVIRAL VECTOR RE-DOSING SCHEDULES FOR IMPROVED AND SUSTAINED TRANSGENE EXPRESSION. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY. |
| 2018 | Donnelley, M., & Parsons, D. (2018). HOW DO WE KNOW IF CYSTIC FIBROSIS LUNG GENE THERAPY WORKS? THE IMPORTANCE OF THE RIGHT ANIMAL MODEL, AND THE RIGHT MEASUREMENT METHOD. Poster session presented at the meeting of JOURNAL OF GENE MEDICINE. Univ Technol Sydney, Sydney, AUSTRALIA: WILEY. |
| 2018 | Donnelley, M., Klein, M., Hausermann, D., Hall, C., Maksimenko, A., Morgan, K., & Parsons, D. (2018). Non-invasive mucociliary transit assessment in live pig trachea. Poster session presented at the meeting of Abstracts of The Australia & New Zealand Society of Respiratory Science and The Thoracic Society of Australia and New Zealand (ANZSRS/TSANZ) Annual Scientific Meeting 2017, as published in Respirology. Adelaide, Australia: Wiley. DOI |
| 2018 | Mcintyre, C., Donnelley, M., Cmielewski, P., & Parsons, D. (2018). GENERATION OF NEW CYSTIC FIBROSIS RAT MODELS IN AUSTRALIA. Poster session presented at the meeting of RESPIROLOGY. WILEY. |
| 2018 | Carpentieri, C., Farrow, N., Mcintyre, C., Cmielewski, P., Rout-Pitt, N., Parsons, D., & Donnelley, M. (2018). COMPARATIVE EFFICIENCY OF HA AND VSV-G PSEUDOTYPED LENTIVIRAL VECTORS FOR CYSTIC FIBROSIS AIRWAY GENE THERAPY. Poster session presented at the meeting of RESPIROLOGY. WILEY. |
| 2018 | Farrow, N., Cmielewski, P., Donnelley, M., Bertoncello, I., & Parsons, D. (2018). DOES EPITHELIAL ABLATION IN THE NASAL AIRWAYS OF MICE IMPROVE STEM CELL ENGRAFTMENT?. Poster session presented at the meeting of RESPIROLOGY. WILEY. |
| 2018 | Carpentieri, C., Farrow, N., Cmielewski, P., McIntyre, C., McCarron, A., Rout-Pitt, N., . . . Donnelley, M. (2018). Airway Gene-Addition Therapy for Cystic Fibrosis: the VSV-G Pseudotype Produces Higher Transduction Levels Than HA. Poster session presented at the meeting of MOLECULAR THERAPY. Chicago, IL: CELL PRESS. |
| 2018 | Farrow, N., Cmielewski, P., Donnelley, M., Rout-Pitt, N., Bertoncello, I., & Parsons, D. (2018). Epithelial Disruption Enables Human Airway Stem Cell Transplantation in Mouse Nasal Airways. Poster session presented at the meeting of MOLECULAR THERAPY. Chicago, IL: CELL PRESS. |
| 2018 | Werdiger, F., Donnelley, M., Parsons, D., Morgan, K. S., Samarage, C. R., Carnibella, R., & Fouras, A. (2018). QUANTIFICATION OF REGIONAL LUNG DISEASE IN β-ENAC MICE USING A LABORATORY X-RAY SOURCE. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY. |
| 2018 | McIntyre, C., Rout-Pitt, N., Donnelley, M., & Parsons, D. (2018). LOBE SPECIFIC TARGETING OF LENTIVIRAL VECTOR GENE TRANSFER TO THE LUNGS OF ADULT RATS. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY. |
| 2018 | McIntyre, C., Cmielewski, P., Craig, F., Rout-Pitt, N., Parsons, D., & Donnelley, M. (2018). CF-RELATED PATHOLOGIES ARE MORE SEVERE IN KNOCKOUT RATS COMPARED TO PHE508DEL RATS. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY. |
| 2017 | Farrow, N., Donnelley, M., McIntyre, C., Rout-Pitt, N., & Parsons, D. (2017). Developing high efficiency gene transfer techniques using human air liquid interface cultures. Poster session presented at the meeting of TSANZ Poster presentations, as published in Respirology. Canberra: Wiley. |
| 2017 | McCarron, A., Rout-Pitt, N., McIntyre, C., Donnelley, M., & Parsons, D. W. D. (2017). Lentivirus Production in Stirred-Tank and Packed-Bed Basket Bioreactor Systems: A Comparison. Poster session presented at the meeting of MOLECULAR THERAPY. Washington, DC: CELL PRESS. |
| 2017 | Farrow, N., Donnelley, M., Rout-Pitt, N., McIntyre, C., Bertoncello, I., & Parsons, D. W. D. (2017). High Efficiency <i>In Vitro</i> Transduction of Human Airway Basal Cells. Poster session presented at the meeting of MOLECULAR THERAPY. Washington, DC: CELL PRESS. |
| 2017 | Farrow, N., Cmielewski, P., Donnelley, M., & Parsons, D. (2017). HIGH EFFICIENCY LENTIVIRAL HUMAN AIRWAY BASAL CELL TRANSDUCTION. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY. |
| 2017 | Carpentieri, C. L., Farrow, N., McIntyre, C., McCarron, A., Rout-Pitt, N., Parsons, D., & Donnelley, M. (2017). COMPARATIVE EFFICIENCY OF HA AND VSV-G PSEUDOTYPED LENTIVIRAL VECTORS DEVELOPED FOR TREATING CYSTIC FIBROSIS LUNG DISEASE. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY. |
| 2017 | Werdiger, F., Murrie, R., Kitchen, M., Samarage, C., Carnibella, R., Fouras, A., . . . Parsons, D. (2017). Detection of regional lung disease in β-ENaC mice on a laboratory x-ray source. Poster session presented at the meeting of Abstracts of the 31st Annual North American Cystic Fibrosis Conference, as published in Pediatric Pulmonology. Indianapolis, Indiana: Wiley-Blackwell. DOI |
| 2017 | McIntyre, C., Donnelley, M., Cmielewski, P., & David, P. W. (2017). Generation of new cystic fibrosis rat models in Australia developed using CRISPR/Cas9 genome editing. Poster session presented at the meeting of Pediatric Pulmonology. Indianapolis, Indiana: Wiley. DOI WoS1 |
| 2016 | Donnelley, M., Morgan, K., & Parsons, D. W. (2016). DIRECT X-RAY MEASUREMENT OF AIRWAY SURFACE HEALTH IN ANIMAL MODELS: AN UPDATE ON THE STATE-OF-THE-ART. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY-BLACKWELL. |
| 2015 | McIntyre, C., Craig, F., Cmielewski, P., Donnelley, M., Farrow, N., & Parsons, D. (2015). Comparing the Efficacy of Tat-Dependent and Tat-Independent Lentiviral Vectors. Poster session presented at the meeting of MOLECULAR THERAPY. New Orleans, LA: NATURE PUBLISHING GROUP. DOI |
| 2015 | Devereux, S., Cmielewski, P., Farrow, N., & Parsons, D. (2015). Airway Pre-Treatment Enhances Mouse Lung Lentiviral Reporter Gene Expression. Poster session presented at the meeting of MOLECULAR THERAPY. New Orleans, LA: NATURE PUBLISHING GROUP. DOI |
| 2015 | Kicic, A., Ling, K., Martinovich, K., Garratt, L. W., Looi, K., Kicic-Starcevich, E., . . . Moodley, Y. (2015). CORRECTIVE EFFECTS ON AIRWAY EPITHELIAL FUNCTION BY HUMAN AMNIOTIC EPITHELIAL CELLS (HAEC) WHEN TREATING CYSTIC FIBROSIS. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY-BLACKWELL. |
| 2015 | Farrow, N. R., McQualter, J., Donnelley, M., Cmielewski, P., Bertoncello, I., & Parsons, D. (2015). CYSTIC FIBROSIS MOUSE MODELS DISPLAY AGE DEPENDENT AIRWAY STEM/PROGENITOR CELL HYPERPLASIA. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY-BLACKWELL. |
| 2015 | Cmielewski, P., Parsons, D., Donnelley, M., Padmanabhan, H., Ling, K., Stick, S. M., . . . Moodley, Y. (2015). DELIVERY OF HUMAN AMNIOTIC STEM CELLS CORRECTS CFTR FUNCTION IN CF MOUSE NASAL AIRWAYS IN VIVO. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY-BLACKWELL. |
| 2014 | Farrow, N. R., McQualter, J. L., Donnelley, M., Bertoncello, I., & Parsons, D. W. (2014). GENE THERAPY FOR CF: IS LONG TERM EXPRESSION A CONSEQUENCE OF TRANSDUCING CONDUCTING AIRWAY ENDOGENOUS RESPIRATORY STEM CELLS?. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY-BLACKWELL. |
| 2014 | Cmielewski, P., Farrow, N., McIntyre, C., Padmanabhan, H., Donnelley, M., Kuchel, T., & Parsons, D. W. (2014). Lentiviral Airway Gene Transfer in Normal Ferrets. Poster session presented at the meeting of MOLECULAR THERAPY. Washington, DC: NATURE PUBLISHING GROUP. |
| 2014 | Padmanabhan, H., Cmielewski, P., Donnelley, M., & Parsons, D. (2014). IMPROVING THE TRANSDUCTION EFFICIENCY OF AN AEROSOL DELIVERED LENTIVIRAL VECTOR FOR CYSTIC FIBROSIS LUNG GENE THERAPY. Poster session presented at the meeting of JOURNAL OF AEROSOL MEDICINE AND PULMONARY DRUG DELIVERY. MARY ANN LIEBERT, INC. |
| 2014 | Stahr, C. S., Samarage, C. R., Parsons, D. W., Dubsky, S., Donnelley, M., Thurgood, J., . . . Fouras, A. (2014). Regional Image Based Pulmonary Function Testing Detects Cf Lung Disease Earlier Than Conventional Pft. Poster session presented at the meeting of AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE. AMER THORACIC SOC. |
| 2013 | Morgan, K., Donnelley, M., Fouras, A., Siu, K., & Parsons, D. (2013). Changes in airway surface liquid depth imaged after aerosolized hypertonic saline. Poster session presented at the meeting of Abstracts of the Thoracic Society of Australia & New Zealand and the Australian & New Zealand Society of Respiratory Science 2013 Annual Scientific Meetings, as published in Respirology. Darwin, N.T.: Wiley-Blackwell. DOI |
| 2013 | Donnelley, M., Morgan, K. S., Siu, K. K. W., Farrow, N., Chua, C., Fouras, A., & Parsons, D. (2013). In-vivo changes in mucociliary transport after aerosols. Poster session presented at the meeting of Abstracts of the Thoracic Society of Australia & New Zealand and the Australian & New Zealand Society of Respiratory Science 2013 Annual Scientific Meetings, as published in Respirology. Darwin, N.T.: Wiley-Blackwell. DOI |
| 2012 | Morgan, K. S., Donnelley, M., Fouras, A., Parsons, D., & Siu, K. (2012). SYNCHROTRON PHASE CONTRAST X-RAY IMAGING CAN DETECT AIRWAY SURFACE LIQUID DEPTH CHANGES FOLLOWING AEROSOLISED HYPERTONIC SALINE TREATMENT. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY-BLACKWELL. |
| 2012 | Siu, K., Chua, C. S., Donnelley, M., Morgan, K. S., Farrow, N., Mall, M. A., . . . Fouras, A. (2012). REGIONAL MEASURES OF LUNG FUNCTION IN THE β-ENAC MOUSE OBTAINED USING X-RAY IMAGING VELOCIMETRY. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY-BLACKWELL. |
| 2012 | Donnelley, M., Siu, K., Morgan, K., & Parsons, D. (2012). Distribution, dynamics and variability of fluid doses into live mouse lungs is revealed using high resolution synchrotron X-ray imaging. Poster session presented at the meeting of Abstracts of the 2012 Thoracic Society of Australia & New Zealand and the Australian & New Zealand Society of Respiratory Science Annual Scientific Meetings, as published in Respirology. Canberra, Australia: Wiley-Blackwell. DOI |
| 2012 | Parsons, D., Karen, S., Kaye, M., & Donnelley, M. (2012). High Speed X-Ray Imaging Reveals Dosed Fluid Dynamics and Fate in Mouse Nasal and Lung Airways. Poster session presented at the meeting of MOLECULAR THERAPY. Philadelphia, PA: NATURE PUBLISHING GROUP. |
| 2012 | Donnelley, M., Siu, K., Morgan, K., & Parsons, D. (2012). HIGH FRAME RATE IMAGING OF NASAL FLUID DOSING DYNAMICS. Poster session presented at the meeting of RESPIROLOGY. WILEY-BLACKWELL. |
| 2011 | Donnelley, M., Siu, K. K., Morgan, K. S., & Parsons, D. W. (2011). DRY DEPOSITION OF POLLUTANT AND MARKER PARTICLES ONTO LIVE MOUSE AIRWAY SURFACES REVEALS HETEROGENEOUS MUCOCILIARY TRANSIT BEHAVIOUR. Poster session presented at the meeting of PEDIATRIC PULMONOLOGY. WILEY-BLACKWELL. |
| 2009 | Donnelley, M. W., Morgan, K., Fouras, A., Skinner, W., Uesugi, K., Yagi, N., . . . Parsons, D. W. (2009). Individual particulate mucociliary transit analysis using synchrotron X-ray imaging. Poster session presented at the meeting of Abstracts of the 23rd Annual North American Cystic Fibrosis Conference, as published in Pediatric Pulmonology. Minneapolis, Minn.: Wiley-Liss. DOI |
| Year | Citation |
|---|---|
| - | Smith, R., Carron, A. M., Donnelley, M., Parsons, D., Morgan, K., Reyne, N., & Cmielewski, P. (n.d.). Directional Dark-Field Imaging Data of Magnet Assisted Airway Treatment Delivery. DOI |
| - | Smith, R., Donnelley, M., Reyne, N., Cmielewski, P., & Parsons, D. (n.d.). X-ray Velocimetry and flexivent measurements of Cystic Fibrosis rat models before and after a localised insult to the lung. DOI |
| - | Smith, R., Donnelley, M., Reyne, N., ASSELIN-LABAT, M. -L., & Batey, D. (n.d.). X-ray Velocimetry, CT, Flexivent and Histology dataset of mice with lung tumours.. DOI |
| - | Smith, R., Donnelley, M., Parkinson-Lawrence, E., & Orgeig, S. (n.d.). X-ray Velocimetry and Flexivent data for a cohort of mice with Mucopolysaccharidosis type I (MPS I) disease. DOI |
| - | Smith, R., Donnelley, M., Nguyen, P., & Badiei, A. (n.d.). X-ray Velocimetry and CT images of healthy sheep undergoing endobronchial valve placement and removal. DOI |
| - | Smith, R., Donnelley, M., Reyne, N., & Mall, M. A. (n.d.). X-ray Velocimetry and Flexivent data for a cohort of the Beta-ENaC-TG mouse model of Cystic Fibrosis. DOI |
| Year | Citation |
|---|---|
| 2025 | Smith, R., Reyne, N., Batey, D., Eikelis, N., Asselin Labat, M. -L., & Donnelley, M. (2025). Mapping Lung Cancer Ventilation Dynamics: A Pilot Mouse Study Using Functional Imaging and Lung Mechanics. DOI |
| 2025 | Rout-Pitt, N., Barnes, S., Reyne, N., McCarron, A., Donnelley, M., Kostecki, R., & Noschka, E. (2025). Evaluating an In Vivo Oxidative Stress sensor in cystic fibrosis rat epithelial tissues. DOI |
| 2024 | Harker, S., Preissner, M., Chang, R. Y., Trevascus, D., Liu, C., Wang, Y., . . . Morgan, K. (2024). Using X-ray Velocimetry to measure lung function and assess the efficacy of a Pseudomonas aeruginosa bacteriophage therapy for cystic fibrosis. DOI |
| 2024 | McCarron, A., Ling, K. -M., Montgomery, S., Martinovich, K., Cmielewski, P., Rout-Pitt, N., . . . Donnelley, M. (2024). Lentiviral vector gene therapy and CFTR modulators show comparable effectiveness in cystic fibrosis rat airway models. DOI |
| 2024 | Reyne, N., Smith, R., Cmielewski, P., Eikelis, N., Nilsen, K., Louise, J., . . . Donnelley, M. (2024). Functional lung imaging identifies peripheral ventilation changes in mice with muco-obstructive lung disease. DOI |
2027-30 M. Donnelley, A. Tai, D. Dharmaprani, R. Smith, N. Reyne, D. Parsons, J. Louise, N. Eikelis, NHMRC Ideas Grant GNT2046960, “Improving Paediatric Respiratory Outcomes Using X-ray Velocimetry Functional Imaging”, $1,949,781
2026-27 S. Liu, M. Donnelley, T. Goddard, Cure4CF Foundation Holckner Family Impact Grant: “A Targeted Novel Therapy for Cystic Fibrosis Lung Infections”, $300,000
2026-27 F. Adikusuma, M. Donnelley, A. McCarron, G. Kaiko, B. Thierry, A. Hussain, P. Thomas, C. Zhao, A. Kicic, S. Woods, Cure4CF Foundation Holckner Family Impact Grant: “Cutting-Edge Gene Editing for Cystic Fibrosis: A Universal One-Time Therapy”, $295,000
2026-29 M. Donnelley, A. Tai, K. Carson-Chahhoud, D. Parsons, D. Dharmaprani, R. Smith, N. Reyne, N. Eikelis, R. Gray, A. Fouras, J. Louise, MRFF Chronic Respiratory Conditions Grant MRF2045660, “Transforming Paediatric Respiratory Care with X-ray Velocimetry Functional Lung Imaging”, $1,836,698 (Relinquished)
2025-27 M. Donnelley, T. O'Meara, D. Dharmaprani, K. Ehinger, T Drummond, Australia's Economic Accelerator Innovate Grant IV240100090: “Commercialisation of novel AI-assisted functional imaging technologies for understanding lung disease”, $3,791,636
2025 N. Rout-Pitt, A. McCarron, N. Reyne, D. Parsons, M. Donnelley, ACFRT Conquer CF Gene Therapy Innovation Grant: “Improving CFTR gene therapy by ensuring airway cells exist in an epithelial state”, $80,000
2025 A. McCarron, N. Rout-Pitt, N. Reyne, D. Parsons, M. Donnelley, ACFRT Conquer CF Gene Therapy Innovation Grant: “Delivery: the final barrier to overcome for effective cystic fibrosis airway gene therapy”, $80,000
2025 J. Darby, J. Morrison, M. Stark, M. Donnelley, D. Parsons, M. Wiese, A. Meakin, M. Lock, Channel 7 Children's Research Foundation Grant: “Turning off the danger signal: reducing ventilator induced lung injury in preterm infants”, $100,000
2024 N. Rout-Pitt, A. McCarron, N. Reyne, S. Waters, M. Donnelley, D. Parsons, USA CF Foundation Grant: “Modifying the airway epithelialmesenchymal state to enhance the effectiveness of CF lung therapeutics”, $162,697
2024 A. McCarron, K. Morgan, D. Parsons, M. Donnelley, R. Smith, Australian Cystic Fibrosis Research Trust Innovation Grant: “Harnessing the power of magnets: Improved effectiveness of airway gene therapy for the treatment of cystic fibrosis lung disease”, $80,000
2024 J. Darby, J. Morrison, M. Stark, M. Donnelley, D. Parsons, M. Wiese, A. Meakin, Channel 7 Children's Research Foundation Grant: “A novel prophylactic for the prevention of ventilator induced lung injury in preterm infants”, $100,000
2024 E. Parkinson-Lawrence, N. Shlezinger, S. Orgeig, M. Donnelley, D. Parsons, A. Tai, D. Brooks, S. Selemidis, J. Logan, S. Bailey, Sanfilippo Children's Foundation Grant: “Repurposing immunomodulatory drugs for the treatment of recurrent lung infections in the challenged Mucopolysaccharidosis type IIIA (MPS IIIA or Sanfilippo syndrome) mouse lung”, $90,880
2024-25 E. Schneider-Futschik, M. Habgood, D. Parsons, M. Donnelley, USA CF Foundation Grant: “Delaying the onset of cystic fibrosis lung pathologies”, $245,000
2023-24 A. McCarron, N. Reyne, P. Cmielewski, M. Donnelley, D. Parsons, Channel 7 Children's Research Foundation Grant: “Does the presence of lung infection impact the efficacy of cystic fibrosis airway gene therapy?”, $40,060
2022 E. Parkinson-Lawrence, S. Orgeig, M. Donnelley, D. Parsons, J. Logan, D. Brooks, MPS Foundation Grant: “Quantification of airway disease in MPS 1 mice via laboratory X-ray velocimetry”, $68,380
2021 M. Donnelley, D. Parsons, A. McCarron, T. Goddard, C. Christou, USA CF Foundation Grant: “Effective delivery of genetic therapeutics for cystic fibrosis airway disease”, $415,000
2021 E. Schneider-Futschik, M. Habgood, D. Parsons, M. Donnelley, Australian Cystic Fibrosis Research Trust Innovation Grant: “Safety and effectiveness of triple -caftor combinations in cystic fibrosis during pregnancy”, $80,000
2021-24 A. Fouras, M. Donnelley, D. Parsons, Australian Lung Health Initiative (4DMedical, University of Adelaide, SAHMRI), MRFF Frontier Health and Medical Research Program Stage Two Grant: “4D Functional Diagnosis: A New Frontier In Lung Health For Children”, $5,285,074
2020 D. Parsons, M. Donnelley, The Hospital Research Foundation Grant: “A simple rapid-production ventilator for COVID-19 treatment applications worldwide”, $25,000
2020 S. Hodge, A. Tai, D. Parsons, M. Donnelley, P. Zalewski, WCH Foundation Grant: “Increased lung artery blood pressure pulmonary hypertension and vascular dysfunction in children with cystic fibrosis”, $100,000
2020 A. McCarron, M. Donnelley, P. Cmielewski, D. Parsons, WCH Foundation Grant: “Airway gene correction in neonatal cystic fibrosis rats”, $100,000
2019 S. Vreugde, D. Parsons, M. Donnelley, K. Inthavong, P. Wormald, National Foundation For Medical Research and Innovation Grant: “A novel treatment for Non-Tuberculous Mycobacteria lung infections in cystic fibrosis patients”, $175,000
2020-23 A. Juhasz, T. Kuchel, D. Parsons, M. Donnelley, T. Prow, NHMRC PFAS Targeted Call 1186337: “Impact of exposure pathway and source on PFAS absorption and bioavailability”, $1.4M
2019 Assisted with the writing of, and lobbying for, a National Imaging Facility Bid to establish small and large animal function lung imaging equipment at the SAHMRI Gilles Plains facility, $4.8M
2019 Australian Lung Health Initiative, MRFF Frontier Health and Medical Research Program Stage One Grant: “4D Functional Diagnosis: A New Frontier In Lung Health For Children”, $960,000
2019 N. Farrow, M. Donnelley, A. Jaffe, D. Parsons, S. Waters, Orphan Disease Center Pilot Grant: “Airway Cell Therapy for Cystic Fibrosis Nonsense Mutations”, $73,000
2019-22 D. Parsons, M. Donnelley, K. Morgan, R. Boucher, T. Kuchel, NHMRC Project Grant: “Translating cystic fibrosis gene-addition therapy for use in human lungs: Demonstrating efficacy, safety and scalability”, $861,345
2019 N. Rout-Pitt, N. Farrow, J. Delhove, D. Parsons, M. Donnelley, WCH Foundation Grant: “Cell plasticity of the airways: Understanding the stem cell niche to optimise gene therapy and stem cell targeting”, $75,000
2019 J. Delhove, M. Donnelley, N. Farrow, D. Parsons, WCH Foundation Grant: “Designing immune-stealth, antiphagocytic targeting vectors for cystic fibrosis lentiviral gene therapy”, $75,000
2019 N. Farrow, M. Donnelley, P. Cmielewski, J. Delhove, D. Parsons, Channel 7 Childrens Research Foundation Grant: “Can neonatal exposure improve the effectiveness of cystic fibrosis gene therapy re-dosing?”, $34,625
2018-19 D. Parsons, M. Donnelley, M. Kitchen, K. Morgan, G. Zosky, J. Breen, USA CF Foundation Grant: “Lentiviral CFTR gene-addition in CF rat lungs: Effect of PA infection, safety and efficacy”, $282,491
2018-19 M. Donnelley, D. Parsons, Gandel Philanthropy Major Grant (via the Cure 4 CF Foundation): “An Australian gene therapy designed to cure CF lung disease: pre-clinical development of an essential, game-changing new lung health measurement technique”, $166,000
2018 M. Donnelley, Robinson Research Institute Career Development Fellowship, $50,000
2018 M. Donnelley, N. Farrow, P. Cmielewski, A. McCarron, D. Parsons, WCH Foundation Grant: “Effective re-dosing protocols for lasting cystic fibrosis lentiviral airway gene therapy”, $75,000
2017–18 D. Parsons, M. Donnelley, Fay Fuller Discovery Project Grant (via the Cure 4 CF Foundation): “Can in vivo delivery of the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) gene soon after birth prevent the establishment and / or progression of Cystic Fibrosis (CF) lung disease?”, $670,292
2017 N. Farrow, M. Donnelley, P. Cmielewski, D. Parsons, WCH Foundation Grant: “Quantifying lentiviral mediated gene expression for cystic fibrosis lung disease in normal rat lungs”, $72,975
2017 C. McIntyre, D. Parsons, M. Donnelley, P. Cmielewski, Channel 7 Childrens Research Foundation Grant: “Gene therapy for cystic fibrosis”, $34,412
2017 M. Donnelley, C. McIntyre, N. Rout-Pitt, A. McCarron, D. Parsons, Channel 7 Childrens Research Foundation Grant: “Improving the efficiency of cystic fibrosis airway gene therapy”, $74,213
2016–18 D. Parsons, I. Bertoncello, M. Donnelley, R.Boucher, T. Kuchel, NHMRC Project Grant 1098127: “Identifying the role of airway stem cells in maintaining lentiviral mediated gene expression for cystic fibrosis lung disease”, $814,272
2015 M.Donnelley, K. Morgan, D. Parsons, A. Fouras, I. Lee, WCH Foundation Grant: “Next generation non-invasive airway surface health assessment: Combined surface hydration and mucus clearance analysis for CF treatment development”, $67,824
2015–17 D. Parsons, A. Fouras, J. Li, K. Siu, R. Boucher, K. Morgan, M. Donnelley, M. Kitchen, NHMRC Project Grant 1079712: “Revolutionising the diagnosis and monitoring of CF lung disease”, $792,778
2014 M.Donnelley, D. Parsons, A. Juhasz, E. Smith, K. Morgan, K. Siu, WCH Foundation Grant: “Lead air-pollution in children: Airway surface behaviour of inhaled particles and influence on blood levels”, $69,687
2013–16 M. Donnelley, MS McLeod Postdoctoral Fellowship: “Uptake of inhaled lead: Description and modelling of deposition, and determinants of vascular uptake”, $310,000
2012 M.Donnelley, D. Parsons, K. Siu, A. Fouras, K. Morgan, WCH Foundation Grant: “Understanding the clearance of inhaled lead dust in the conducting airways using synchrotron imaging”, $43,754
2011 D. Parsons, A. Fouras, K. Siu, S. Hooper, M. Donnelley, Australian Cystic Fibrosis Research Trust Grant: “Localised detection of early stage CF disease via quantitative imaging of lung motion”, $110,749
2010–12 D. Parsons, K. Siu, M. Donnelley, W. Skinner, NHMRC Project Grant 626863: “Synchrotron X-ray assessment of airway surface physiology for cystic fibrosis”, $765,702 (Score of 7)
2009 D. Parsons, M.Donnelley, K. Siu, N. Yagi, M. Kitchen, WCH Foundation Grant: “Dynamic synchrotron x-ray detection of individual pollutant particle behaviour after deposition onto live airways”, $54,360
| Date | Role | Research Topic | Program | Degree Type | Student Load | Student Name |
|---|---|---|---|---|---|---|
| 2024 | Principal Supervisor | Developing an effective airway stem cell therapy for the treatment of Cystic Fibrosis lung disease | Doctor of Philosophy | Doctorate | Full Time | Ms Stuti Saini |
| 2024 | Principal Supervisor | Developing an effective airway stem cell therapy for the treatment of Cystic Fibrosis lung disease | Doctor of Philosophy | Doctorate | Full Time | Ms Stuti Saini |
| 2023 | Principal Supervisor | Understanding and improving gene vector targeting with lentiviral magnetic nanoparticles | Doctor of Philosophy under a Jointly-awarded Degree Agreement with | Doctorate | Part Time | Ms Madison Michelle Davis |
| 2023 | Co-Supervisor | Paediatric Regional Lung Function Assessment Via X-Ray Velocimetry In Children With Cystic Fibrosis | Doctor of Philosophy | Doctorate | Part Time | Mr Matthew Russell Bruorton |
| 2023 | Principal Supervisor | Understanding and improving gene vector targeting with lentiviral magnetic nanoparticles | Doctor of Philosophy | Doctorate | Part Time | Ms Madison Michelle Davis |
| 2023 | Co-Supervisor | Paediatric Regional Lung Function Assessment Via X-Ray Velocimetry In Children With Cystic Fibrosis | Doctor of Philosophy | Doctorate | Part Time | Mr Matthew Russell Bruorton |
| Date | Role | Research Topic | Program | Degree Type | Student Load | Student Name |
|---|---|---|---|---|---|---|
| 2021 - 2024 | Principal Supervisor | Novel Tools and Models for In-vivo Assessment of Lung Health in Cystic Fibrosis | Doctor of Philosophy | Doctorate | Full Time | Mrs Nikki Reyne |
| 2016 - 2021 | Co-Supervisor | Overcoming Challenges to Development of a Lentiviral-Mediated Airway Gene-Addition Therapy for Cystic Fibrosis | Doctor of Philosophy | Doctorate | Full Time | Miss Alexandra Sarah Ann Mc Carron |
| 2013 - 2019 | Co-Supervisor | Development of Lentiviral Airway Gene Therapy Aerosol Delivery Techniques for Cystic Fibrosis | Doctor of Philosophy | Doctorate | Full Time | Ms Harshavardini Padmanabhan |
| Date | Role | Committee | Institution | Country |
|---|---|---|---|---|
| 2022 - ongoing | Chair | Micro-Computed Tomography beamline Program Access Committee | Australian Synchrotron | Australia |
| 2022 - ongoing | Member | Respiratory and GI tract Committee | American Society of Gene and Cell Therapy | United States |
| 2021 - ongoing | Chair | Imaging and Medical Beamline Program Access Committee | Australian Synchrotron | Australia |
| 2020 - ongoing | Member | Animal Ethics Committee (Medical) | University of Adelaide | Australia |
| 2017 - 2018 | Member | Annual Symposium Planning Committee | Robinson Research Institute | Australia |
| 2016 - 2018 | Member | Early and Mid Career Research Council | Robinson Research Institute | Australia |
| 2015 - 2018 | Chair | Scientists Special Interest Group | Australasian Cystic Fibrosis Conference | Australia |
| Date | Role | Membership | Country |
|---|---|---|---|
| 2018 - ongoing | Member | American Society of Gene and Cell Therapy | United States |
| 2018 - ongoing | Member | Australian and New Zealand Society of Respiratory Science | Australia |
| 2001 - ongoing | Member | Institute for Electrical and Electronic Engineers | United States |
| Date | Role | Editorial Board Name | Institution | Country |
|---|---|---|---|---|
| 2020 - ongoing | Editor | Scientific Reports | Nature | United Kingdom |
| 2020 - ongoing | Board Member | Gene Therapy (Basingstoke) | Nature | United Kingdom |
| 2020 - ongoing | Board Member | Respiratory Research | BMC | United Kingdom |
| 2019 - ongoing | Board Member | Human Gene Therapy | Mary Anne Liebert | United States |











Available For Media Comment.