Mr Sabapathy Krishnan
School of Medicine
College of Health
Eligible to supervise Masters and PhD - email supervisor to discuss availability.
Dr Giri Krishnan is an Otolaryngology, Head and Neck Surgical trainee. He completed his medical degree at The University of Adelaide in 2013 and a Master of Clinical Science at the Joanna Briggs Institute in 2017. He is currently undertaking a PhD as part of a 'Surgeon-Scientist Training Program' investigating the application of novel nanoparticles to advance diagnosis and treatment of patients with head and neck cancer. Giri was awarded the 2018 Fulbright scholarship, and will undertake a research fellowship, as part of his PhD, at Stanford University in California, USA in 2019. He will work in the Rosenthal Laboratory where he will have access to state of the art preclinical imaging facilities. He aims to use advanced magnetic nanotracers for molecular imaging to identify microscopic metastatic cancer deposits in a mouse head and neck cancer xenograft model and study the use of fluorescent probes for real-time optical imaging during head and neck surgery.
My PhD investigates the role of nanotechnology to advance diagnosis and treatment of patients with head and neck cancer. This research brings together a team of expert South Australian Head and Neck Surgeons from the Royal Adelaide Hospital with Bioengineers from the Future Industries Institute and scientists from the Basil Hetzel Institute to translate cutting-edge and innovative nanoparticle technology into clinical practice. My supervisors are Professor PJ Wormald, Professor Benjamin Thierry and Dr. Andrew Foreman.
Oral cancer is the 12th most common cancer in the world and contributes a significant public health burden because of the aggressive nature of this disease and its associated poor patient survival outcomes.

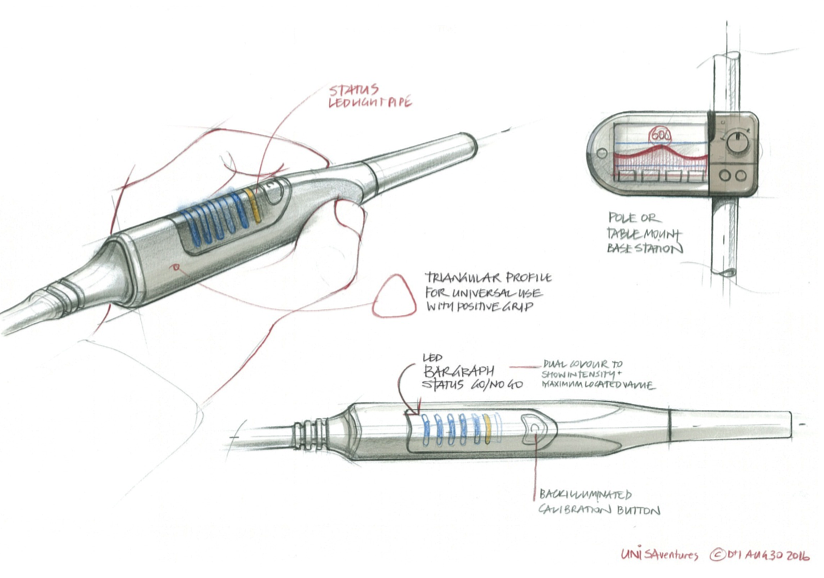
Nanoparticles offer several exciting opportunities in oral cancer research. Nanoparticles can be used as ‘tracers’ to help us detect the spread of microscopic cancer in imaging studies, by labelling them with immune antibodies that are specifically attracted to cancer cells. Accurate detection of cancer is critical because a missed diagnosis portends an extremely poor prognosis. They can also be used in a therapeutic fashion. For example they can be designed to deliver chemotherapeutic drugs directly to the tumour, reducing the systemic toxic effects of therapy. In a similar fashion they can be used for “radiosensitisation” of tumours by enhancing the effects of radiotherapy on the tumour. My team have manufactured magnetic nanotracers and have designed a unique hand-held 'magnetometer probe' that will enable us to perform sentinel lymph node mapping using a novel magnetic technique in the head and neck to identify the regional spread of tumour to the lymph nodes in the neck.
The specific objectives of my PhD are to initially develop a small animal model of oral cancer and then to explore in this model, the feasibility of using advanced nanoparticles in each of these innovative diagnostic and treatment strategies. I will work with our team of experienced Head and Neck Surgeons to trial these treatment strategies in human patients.
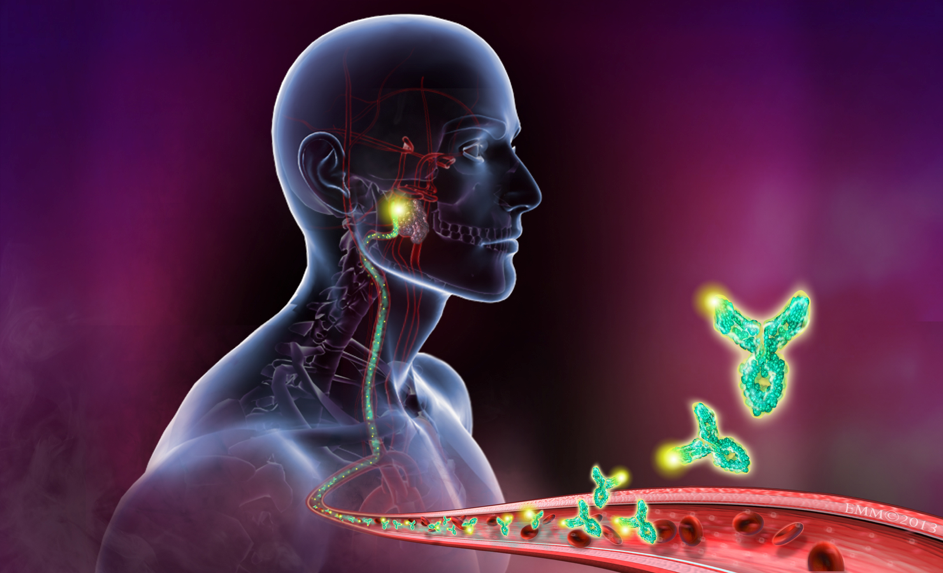
As part of my PhD I will also spend 12 months at Stanford under the supervision of Professor Eben Rosenthal analysing the role of nanoparticles for “real-time optical image guided surgery”. This emerging technique involves labeling nanoparticles with a fluorescent tag, which binds to cancer cells so that we can visualize the tumour margins during surgical resection. This improves our chances of complete tumour clearance, which we know gives our patients a much better chance of survival.
Realisation of our aims could revolutionise the treatment paradigm of our patients giving them more efficient and accurate diagnoses and improving the success, while reducing the associated morbidity, of our medical, radiotherapeutic and surgical treatment.
| Date | Position | Institution name |
|---|---|---|
| 2015 - 2018 | Clinical Associate Lecturer | University of Adelaide, Adelaide |
| Date | Institution name | Country | Title |
|---|---|---|---|
| 2017 | University of Adelaide, Adelaide | Australia | PhD |
| 2015 - 2017 | University of Adelaide, Adelaide | Australia | MClinSc |
| 2007 - 2013 | University of Adelaide, Adelaide | Australia | MBBS |
| Date | Title | Institution | Country |
|---|---|---|---|
| 2018 | Otolaryngology, Head and Neck Surgery Surgical Education Training | Royal Australasian College of Surgeons | Australia |
| 2015 - 2017 | Surgical Residency | Royal Adelaide Hospital, Adelaide | Australia |
| 2014 - 2015 | Internship | Royal Adelaide Hospital, Adelaide | Australia |
| Year | Citation |
|---|---|
| 2023 | Muecke, T., Kovoor, J., Krishnan, G., Bacchi, S., & Chan, W. O. (2023). In Response to Social Media Utilization in Otolaryngology: A Scoping Review.. The Laryngoscope, 133(10), E58-E59. |
| 2022 | Krishnan, G., van den Berg, N. S., Nishio, N., Kapoor, S., Pei, J., Freeman, L., . . . Rosenthal, E. L. (2022). Fluorescent Molecular Imaging Can Improve Intraoperative Sentinel Margin Detection in Oral Squamous Cell Carcinoma. Journal of Nuclear Medicine, 63(8), 1162-1168. Scopus28 WoS29 Europe PMC24 |
| 2022 | Krishnan, G., Cousins, A., Pham, N., Milanova, V., Nelson, M., Krishnan, S., . . . Thierry, B. (2022). Preclinical evaluation of a mannose-labeled magnetic tracer for enhanced sentinel lymph node retention in the head and neck. Nanomedicine: Nanotechnology, Biology and Medicine, 42, 102546-1-102546-11. Scopus9 WoS8 Europe PMC7 |
| 2022 | Krishnan, G., Cousins, A., Pham, N., Milanova, V., Nelson, M., Krishnan, S., . . . Krishnan, S. (2022). Preclinical feasibility of robot-assisted sentinel lymph node biopsy using multi-modality magnetic and fluorescence guidance in the head and neck. Head and Neck, 44(12), 2696-2707. Scopus5 WoS3 Europe PMC4 |
| 2021 | Lee, Y. J., Krishnan, G., Nishio, N., van den Berg, N. S., Lu, G., Martin, B. A., . . . Rosenthal, E. L. (2021). Intraoperative Fluorescence-Guided Surgery in Head and Neck Squamous Cell Carcinoma. Laryngoscope, 131(3), 529-534. Scopus36 WoS30 Europe PMC25 |
| 2021 | Pei, J., Juniper, G., van den Berg, N. S., Nisho, N., Broadt, T., Welch, A. R., . . . Rosenthal, E. L. (2021). Safety and Stability of Antibody-Dye Conjugate in Optical Molecular Imaging. Molecular Imaging and Biology, 23(1), 109-116. Scopus10 Europe PMC10 |
| 2021 | Kapoor, S., Lu, G., van den Berg, N. S., Krishnan, G., Pei, J., Zhou, Q., . . . Nishio, N. (2021). Effect of Formalin Fixation for Near-Infrared Fluorescence Imaging with an Antibody-Dye Conjugate in Head and Neck Cancer Patients. Molecular Imaging and Biology, 23(2), 270-276. Scopus5 Europe PMC6 |
| 2021 | Krishnan, G., van den Berg, N. S., Nishio, N., Juniper, G., Pei, J., Zhou, Q., . . . Rosenthal, E. L. (2021). Metastatic and sentinel lymph node mapping using intravenously delivered Panitumumab-IRDye800CW. Theranostics, 11(15), 7188-7198. Scopus35 Europe PMC23 |
| 2020 | Hart, Z. P., Nishio, N., Krishnan, G., Lu, G., Zhou, Q., Fakurnejad, S., . . . Baik, F. M. (2020). Endoscopic fluorescence-guided surgery for sinonasal cancer using an antibody-dye conjugate. Laryngoscope, 130(12), 2811-2817. Scopus19 WoS18 Europe PMC15 |
| 2020 | Fakurnejad, S., Krishnan, G., van Keulen, S., Nishio, N., Birkeland, A. C., Baik, F. M., . . . Martin, B. A. (2020). Intraoperative Molecular Imaging for ex vivo Assessment of Peripheral Margins in Oral Squamous Cell Carcinoma. Frontiers in Oncology, 9, 7 pages. Scopus33 |
| 2019 | Krishnan, G., Mintz, J., Foreman, A., Hodge, J., & Krishnan, S. (2019). The acceptance and adoption of transoral robotic surgery in Australia and New Zealand. Journal of Robotic Surgery, 13(2), 301-307. Scopus22 WoS18 Europe PMC11 |
| 2019 | Krishnan, G., Stepan, L., Du, C., Padhye, V., Bassiouni, A., Dharmawardana, N., . . . Krishnan, S. (2019). Tonsillectomy using the BiZact: A pilot study in 186 children and adults. Clinical Otolaryngology, OnlinePubl(3), 4 pages. Scopus20 WoS18 Europe PMC12 |
| 2018 | Krishnan, G. (2018). Evolution of neck dissections performed in conjunction with transoral robotic surgery lateral oropharyngectomy. Australian Journal of Otolaryngology, 1(1), 0. Scopus8 |
| 2017 | Krishnan, G., Du, C., Fishman, J., Foreman, A., Lott, D., Farwell, G., . . . Birchall, M. (2017). The current status of human laryngeal transplantation in 2017: A state of the field review. Laryngoscope, 127(8), 1861-1868. Scopus33 WoS22 Europe PMC16 |
| 2017 | Krishnan, G., & Krishnan, S. (2017). Transoral Robotic Surgery Total Laryngectomy: Evaluation of Functional and Survival Outcomes in a Retrospective Case Series at a Single Institution. ORL, 79(4), 191-201. Scopus29 WoS27 Europe PMC22 |
| 2016 | Kao, S. S. T., Peters, M. D. J., Krishnan, S. G., & Ooi, E. H. (2016). Swallowing outcomes following primary surgical resection and primary free flap reconstruction for oral and oropharyngeal squamous cell carcinomas: a systematic review. Laryngoscope, 126(7), 1572-1580. Scopus48 WoS39 Europe PMC33 |
| 2016 | Krishnan, S., Umapathysivam, K., Lockwood, C., & Hodge, J. (2016). Oncological and survival outcomes following transoral robotic surgery versus transoral laser microsurgery for the treatment of oropharyngeal squamous cell carcinoma: a systematic review protocol. JBI database of systematic reviews and implementation reports, 14(8), 90-102. Scopus2 Europe PMC1 |
| Date | Years | Funding Body | Amount |
|---|---|---|---|
| 2018 | 1 | The Fulbright Post-Graduate Scholarship | $35,000 |
| 2018 | 3 | The Garnett Passe and Rodney William’s Foundation Academic Surgeon Scientist Scholarship | $210,000 |
| 2018 | 3 | The Garnett Passe and Rodney Williams Memorial Foundation Conjoint Grant | $300,000 |
| 2018 | 1 | The Australia and New Zealand Head and Neck Cancer Society (ANZHNCS) Research Grant | $5,000 |
| 2017 | 1 | AVANT Doctors in training Advancement of Medicine Scholarship | $50,000 |
| 2017 | 1 | The University of Adelaide, Faculty of Health Sciences Divisional Scholarship | $26,000 |
| 2012 | 6 wks | The University of Adelaide Summer Research Scholarship | $500 |
Courses Summary
Giri is a Clinical Associate Lecturer at the University of Adelaide. He has been involved in teaching a variety of courses and has also be an oral assessor for entry into the medical program as well as an examiner for the medical student clinical examinations.
| Year | Course Title | Institution | School / Department |
|---|---|---|---|
| 2018 | Applied Clinical Anatomy | University of Adelaide | Health Sciences |
| 2017 | Case Based Collaborative Learning | University of Adelaide | Medicine |
| 2016 | Suturing Tutorials | The Royal Adelaide Hospital | Surgery |
| 2015 | Introduction to ENT Course for Interns and Residents | The Royal Adelaide Hospital | Otolaryngology, Head and Neck Surgery |
| 2014 | Bedside Tutorials | The Royal Adelaide Hospital | Medical Education |
| Date | Role | Research Topic | Program | Degree Type | Student Load | Student Name |
|---|---|---|---|---|---|---|
| 2021 - 2023 | Co-Supervisor | Effectiveness Of Reduced Versus Standard Dose Radiation Therapy On Survival And Radiation Associated Toxicity In Human Papillomavirus (HPV) Associated Oropharyngeal Squamous Cell Carcinoma (OPSCC) | Master of Clinical Science | Master | Full Time | Mr Timothy James Lee |
| Date | Role | Membership | Country |
|---|---|---|---|
| 2018 - ongoing | Member | Australian Society of Otolaryngology Head and Neck Surgery | Australia |
| 2018 - ongoing | Member | Royal Australian College of Surgeons | Australia |
| 2017 - ongoing | Member | Australia and New Zealand Head and Neck Society | Australia |
| 2016 - ongoing | Board Member | DREAMIN Foundation Incorporated | - |
| 2015 - 2016 | President | The Royal Adelaide Hospital Resident Medical Officers' Society | Australia |







